VA ClinicsThe VA Clinic rotation is designed to provide exposure to multiple different subspecialty outpatient clinics. Afternoon clinic is staffed by the 3 residents assigned to each of the following services: VA Senior, VA Clinic and VA LP. Each clinic has a focused subspecialty including General Neurology, Neurodegenerative, Epilepsy, Neuromuscular, Multiple Sclerosis, or Stroke and will have oversight by attendings who are experts in these fields.
1 Week Prior to Rotation
Make sure you have VA access. You need to log in to a VA computer and CPRS at the VA or remotely once per month to retain access. If your account ever becomes disabled, can call the VA Helpdesk at 1-855-673-4357.
For remote access: see instructions on how to sign-up. Consider calling for a PIV exemption or order a personal PIV card reader off of Amazon.
Also make sure you have completed your annual TMS training.
Check your Frenkil clinic schedule to see if you have any LPs scheduled on Monday. (see LP Clinic page for additional information specific to LP clinic). You may also have Frenkil Resident Clinic on Tuesday afternoons and Wednesday mornings.
DAY 1/General daily Routine
You should receive a Tiger message or email from the VA Senior the mornings of Monday, Thursday, and Friday outlining the assignments for the afternoon VA clinics on those days. You should receive the Friday morning discharge and LP clinic schedule via email from Dr. Grimes by Thursday.
If you are free the mornings prior to clinic, you have the option to pre-chart on your assigned patients either in the neurology team room on 4A or at home if you have remote access.
Go to the VA clinic right after midday didactics, as the first patients are typically scheduled at 12:30pm. Rooms are located in the 4B hallway, and your room assignment (Resident 1, 2, or 3) should be posted on the door by the MAs prior to clinic starting.
Use VSE to check and track when your patients are checked in and ready. This system is analagous to the Frenkil Clinic Dot System. If you do not know how to use this, please ask the VA Senior to show you how to set this up prior to clinic. There is typically also a Microsoft Teams group created for each clinic, which you should also have open as the MAs will typically message on there when patients are ready to be seen or have no showed in case there are issues with VSE.
heck which resident is on VA LP- if it is a PGY2 who is not signed off to independently perform LPs, you may be responsible for supervising their VA LPs on Friday if you do not have patients scheduled in discharge clinic.
TEAM STRUCTURE
General/Subspecialty Attending(s): Responsible for staffing all patients. Should be available to physically see all patients with PGY2s, all new patients, and any patient for whom there is concern about management. Attendings will typically sit in the neurology team room or one of the VA clinic rooms while waiting to staff patients.
Residents: Responsible for evaluating and managing all patients. Prior to seeing each patient you should review their chart to determine the disease process that is being treated (reminder while patient may be listed as in the stroke clinic they may have neuropathy or seizures etc) as well as the plan that has been established. Each clinic note should end with a concise plan for which studies should have been completed and need follow up as well as potential next steps in evaluation and management.
There are typically 3 residents assigned to VA Clinic as described above, as well as any rotators. The VA Clinic and LP Clinic residents will typically see the majority of patients when that option is available based on the clinic times, as the VA Senior is still expected to manage all inpatient VA consults during this time. The VA Senior may occasionally be pulled away from clinic for more urgent inpatient consults (details for triaging provided under VA Senior guidelines) and so it is expected that the VA Clinic and LP resident will work together to see all patients that are reassigned in a timely and efficient manner. The VA Senior will be responsible for working with the case managers to help manage the flow and triage of clinic.
All new patients seen will need to be staffed and seen with an attending prior to being sent out of the clinic. For follow up patients the PGY-2 (and any additional providers) is expected to present each case to the attending prior to their leaving the clinic. PGY-3 residents may send follow-up patients out of the clinic and present the cases at the end of clinic or when the attending is free. When in doubt about a patient’s working diagnosis or management, please discuss with an attending before sending the patient out from clinic.
Students: Students may join a resident or attending and should be encouraged to do at least part of the evaluation on their own when possible.
SCHEDULE
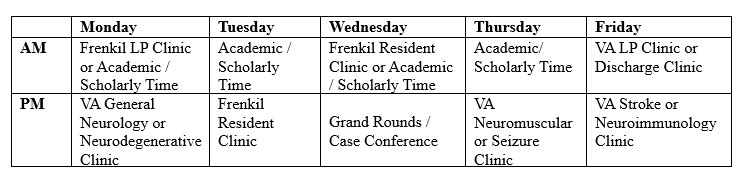
In VA subspecialty clinic on Mondays, Thursdays, and Fridays, residents will see patients as assigned and staff them with the attending. You should receive a Tiger message or email from the VA senior the mornings of Monday, Thursday, and Friday outlining the assignments for the afternoon VA clinic on those days. Afternoon clinics begin at 12:30 PM and you should report as soon as Midday Didactics have finished.
You will also have at least one weekly continuity clinic scheduled at Frenkil during VA clinic. This will be Tuesday afternoon, Wednesday morning, or both.
All residents are expected to be at Morning Report (each day during the summer, Tue/Thu the rest of the year) at 7:45 AM, and at Midday Didactics at 11:30 AM (12:30 AM on Wednesdays).
PATIENT FLOW
Patients arrive to the clinic and check in at the 4A desk.
It is easiest to enter the encounter using the clinic schedule list (BT Neurology Res 1, BT Neurology Res 2, or BT Neurology Res 3 for General, Neurodegenerative, Neuromuscular, Stroke, and Discharge Clinic; BT Seizure or BT New Sz for Seizure Clinic; BT Neuroimmunology Res 1, BT Neuroimmunology Res 2, or BT Neuroimmunology Res 3 for Neuroimmunology Clinic; BT Neu LP for LP Clinic). If you open the chart using the “last initial, last 4 SSN method,” then you will need to manually change the encounter to the correct clinic.
Use VSE to check and track when your patients are checked in and ready. This system is analagous to the Frenkil Clinic Dot System. If you do not know how to use this, please ask the VA Senior to show you how to set this up prior to clinic. There is typically also a Microsoft Teams group created for each clinic, which you should also have open as the MAs will typically message on there when patients are ready to be seen or have no showed in case there are issues with VSE.
Call the patient back to your exam room from the 4A waiting room when you have been notified they are ready (via VSE or Microsoft Teams).
Patients may be marked as a “No Show” if they have not arrived within 30 minutes of their appointment time. Prior to officially marking a No Show, confirm with the MAs via Microsoft Teams to ensure the patient is not in the waiting room. You may be asked to convert the visit to a video visit if the patient does not arrive. If after all of this a patient is a No Show, you will need to write a No Show note.
If you have a telephone or video visit, you may call the patient from an exam room at the stated time.
After you finish evaluating the patient, find the attending to staff prior to completing the visit.
Scheduling follow up visits for a patient should be completed by placing an order for “Return to Clinic” with the specified time frame for their return, and the comment section should include which neurology clinic they should be scheduled in to avoid scheduling patients in the wrong subspecialty clinic. Patients will receive a notification when it is time to schedule their next visit.
Residents are encouraged to determine patient need for follow up. With many stable disease processes (ie prior stroke, diabetic neuropathy, migraine etc) that have had completed work up and do not require a specialist, patients should be discharged back to care of their PCP to return only as needed for additional consultation.
NOTES AND DOCUMENTATION GUIDELINES
It is easiest to enter the encounter using the clinic schedule list (BT Neurology Res 1, BT Neurology Res 2, or BT Neurology Res 3 for General, Neurodegenerative, Neuromuscular, Stroke, and Discharge Clinic; BT Seizure or BT New Sz for Seizure Clinic; BT Neuroimmunology Res 1, BT Neuroimmunology Res 2, or BT Neuroimmunology Res 3 for Neuroimmunology Clinic; BT Neu LP for LP Clinic). If you open the chart using the “last initial, last 4 SSN method,” then you will need to manually change the encounter to the correct clinic prior to starting your note or placing orders.
Clinic notes should all use the templates provided in CPRS or a personal template that you have created. Please speak with the VA Senior for help finding and saving our shared templates. These templates have multiple fields that will autopopulate for you. You will need to remember to add medications and change the exam prior to signing your notes.
**You will need to add the patient data object for Medication Reconciliation to your template for each patient.**
Currently, the clinic is designed as a non-continuity clinic and so you will not necessarily be evaluating any patient a second time in the future. This means that your notes must be very clear in order to ensure appropriate and fluid care for our patients. Each note, especially for follow ups, should concisely identify the course of the patient’s neurologic disease and management. A clear “Assessment and Plan” should be written describing your impressions and thought process for any testing or treatment planned. It is also helpful for your colleagues if you provide a bulleted version of the plan for follow up as well as including a plan for the next visit.
When you begin a note, you will identify the attending that will co-sign your note. You can change this later if needed. After a note has been signed you can right-click the note and select “Identify Additional Signers” in order to add a case manager or PCP that should be notified of your recommendations.
Prior to signing your note, CPRS will take you to the billing page where a level of care, diagnosis and service connection must be completed. The encounter will not be able to be closed without this information.
REQUESTS FOR RESPITE CARE
For inpatient or in home respite---service connection does matter for inpt respite. Also, patients cannot have been in acute care within 30 days before a respite stay.
Inpatient respite is done in the CLCs and is NEVER guaranteed because it depends upon what their bed availability is at the time respite is needed (they CAN cancel it last minute and the family has to be prepared for that possibility). In home respite is HHA service offered for expanded hours for up to 30 days per calendar year.
Usually the SW (typically PACT SW or the primary SW working with the patient) enters those requests and communicates outcomes/feedback to the family.
For in-home respite services it is Nicole Trimble and Nicole Kaiser that would be points of contact and a Community Care In-Home Respite consult has to be entered.
If appropriate for inpatient respite consideration, a GEC screening consult needs to be entered.
TIPS
VA Seniors and PGY-4s are your best resource if you have questions about daily workflow. If issues need to be escalated beyond the resident level, the chiefs and Dr. Savitt are the main point of contact at the VA.
Clinic Schedules are available in CPRS. After logging in, a box will appear in the center of the screen where you can search for patients and see notifications. In the upper left corner of the box there are various lists you can select. Click the one for "Clinics" and search using the clinic lists listed above.
If ordering a MRI, you must complete a checklist or the study will not be scheduled. Go to “BT Add new orders” on the left side menu, and click #37 “MRI.” Once you submit the information, the MRI order will pop up and you can fill it out and sign it.
When ordering consults, please read everything before signing the order! Some services will require certain tests to be performed before they will even consider seeing the patient. Also, there may be some information you are required to fill out at the bottom of the order.
Non-formulary medications require a consult, along with a justification for why the formulary medication is not being requested. These can often get rejected if not correctly worded or filled out. If approved, they are given for 30 days.
For controlled substances, a VA badge is required along with a PIN number.
There is a VA-LP clinic to schedule patients if one is needed. They are done every Friday. Please clearly list in your note what labs you would like sent on the CSF and make sure that CBC and coags are done prior to the patient being scheduled.
GOALS & OBJECTIVES
Be able to evaluate undifferentiated neurological patients, formulate their cases, and propose appropriate diagnostic and therapeutic plans.
Appropriately order and interpret neuroimaging studies.
Counsel patients and families regarding diagnosis and treatment, discuss goals of care, and negotiate conflicts among family/patient and the treatment team.
Clearly and completely document patient care in a timely fashion.
Incorporate feedback and develop a learning plan.
Review literature to incorporate evidence-based medicine in patient care.
Develop appropriate differential and initiate further diagnostic testing and management for movement, neuromuscular, cognitive/behavioral, demyelinating, seizure, neuro-oncologic, and neuropsychiatric/somatoform disorders, along with headache and neurologic manifestation of systemic disease.
Be able to appropriately request consultations from neurologic subspecialists.
Be able to use non-technical terms to explain procedures, such as EEG/EMG.
Last Updated: August 5, 2024