SUBSPECIALTY CLINICs
The subspecialty clinic rotation is designed to ensure residents gain a broad exposure to all neurology subspecialties during their training. The rotation is timed to allow for exposure early in training prior to fellowship decisions, with one week of movement disorders and neuroimmunology each and two weeks of general subspecialty clinic during PGY-2 year.
Subspecialty clinic rotations include
Epilepsy: 4 weeks
Neuromuscular: 4 weeks
General Subspecialty (mix of all subspecialties): 2 weeks
Movement Disorders: 1 week
Neuroimmunology: 1 week
General helpful clinic information can be found on the Continuity Clinic page - please review before your rotation.
For those interested in getting exposure to neuro-ophthalmology: Dr. Singman has offered to have residents shadow him in clinic on 1st and 3rd Tuesdays. If you are interested, please email him directly so that he knows when to expect you: ESingman@som.umaryland.edu. Clinic is held at the Redwood office.
LOCATION
All clinics are held at the Neurology Care Center at 16 S. Eutaw St, 3rd floor except for Neuro-Oncology clinics with Drs. Ahmad and Pham at the Stoler Cancer Pavilion (room varies depending on the day).
SCHEDULE
You will receive a weekly schedule via email.
08:00-11:30 Morning Session
11:30-12:30 Midday Didactics (12:30-1:30 on Wed)*
Residents are excused from midday didactics in leu of subspecialty specific lunchtime meetings when on Neuroimmunology and Movement Rotations
12:30-5:00 Afternoon Session
Each week, the resident will be assigned:
6 Sessions: Subspecialty clinic
1 session Faculty Teaching Practice clinic
1 session Scholarly time (meet with research mentor, work on IRB, analyze data, write, etc.)
1 session Personal time (schedule your own doctor, dentist, car repair, etc.).
Wed Afternoons: Grand Rounds & Case Conference
PLEASE NOTE: If you have your own preferences as to who you want to work with, you must plan ahead and get Courtney this information by Monday of the week before you are scheduled to start your rotation.
You don’t need to have any preferences – if you don’t care what happens and when, do nothing and a schedule will still be made for you.
This is only for general Clinic or Subspecialty rotations, NOT if you are scheduled for the dedicated MS or Movement subspecialty week that is organized by Dr. Fredrich.
If your rotation week contains a holiday, retreat/event day, etc., you should expect that you may have one less personal/scholarly/admin half-day than you normally would. The priority is to make sure that you have time to be with attendings in clinic.
Same rules for personal/scholarly/admin half-days apply as above: if you have a preference as to when that happens, you need to get it to Courtney by the Monday of the week before you are scheduled to start the rotation.
Late requests are left to Courtney’s discretion based on whether or not she has started making the schedule. If you miss the deadline then you may not get what you want.
EVALUATIONS
Ask Penelope Birckhead to send the evaluation for this rotation through MedHub to whichever attending you worked with the most.
This rotation is an opportune time to complete Clinical Skills Exam requirements for ABPN board eligibility. More information on the CSE requirements here.
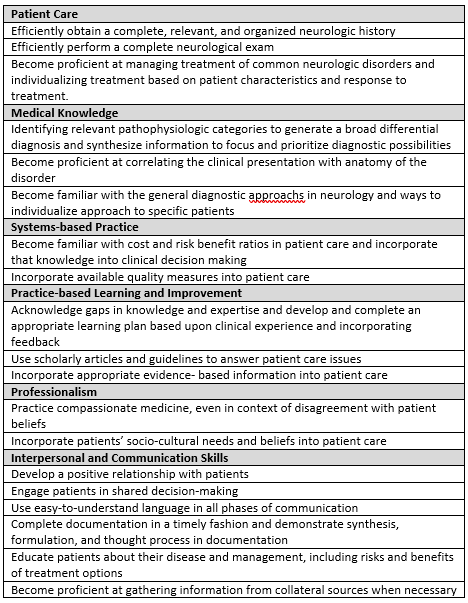
COMPETENCY-BASED GOALS AND OBJECTIVES
SUBSPECIALTY - SPECIFIC INFO
NEURO-IMMUNOLOGY
Learning Objectives
Discuss approaches to MS diagnosis, including the application of the McDonald Criteria, as well as ancillary studies including CSF studies and MRI
Discuss differential diagnosis of demyelinating and other inflammatory CNS disorders
Discuss the clinical features of MS phenotypes
Identification and evaluation of a MS relapse
Discuss evaluation of MS-related disability
Identify and discuss the MS platform disease-modifying therapies
Identify MS treatment failure
Gain experience in decision-making regarding disease-modifying therapy transitions
Gain experience with MS symptom management
Schedule
Unless otherwise specified in the assignment email, the rotation schedule for Neuroimmunology is as below:
Lunchtime Meetings (11:30-12:30pm):
1st and 3rd Thursdays: Case Conference
Bressler Research Building 12th floor conference room
4th Thursdays: Research Meeting
Shock Trauma Conference Room
5th Thursdays: Journal Club
Shock Trauma Conference Room
* = Residents may request >1 week in advance to trade one half day of Dr. Fredrich clinic for OCT Reading with Dr. Harrison, Neuroanatomy and CSF with Dr. Benavides, or Iatrogenic Demyelinating Diseases with Dr. Fredrich. Email the attending of your interest.
^ For those interested in Autoimmune Neurology, residents may request >1 week in advance attendance in the UMCCAN clinic by emailing Dr. Fredrich. There is no UMCCAN on 5th Friday’s.
Readings
AAN Practice Parameters
Disease modifying therapies: https://www.aan.com/Guidelines/home/GuidelineDetail/898
Rehabilitation in MS: https://www.aan.com/Guidelines/home/GuidelineDetail/720
Complementary and Alternative Medicine: https://www.aan.com/Guidelines/home/GuidelineDetail/64
Others:
CONTINUUM: Multiple Sclerosis and Other Demyelinating Diseases.
Reich DS, et al. Multiple Sclerosis. NEJM. 2018 Jan 11;378(2):169-180. [PMID: 29320652]
MOVEMENT DISORDERS
Learning Objectives
Perform a thorough and accurate neurologic history and examination on an adult patient with a Movement Disorder.
Initiate the appropriate diagnostic evaluation of most patients who present with both common and uncommon Movement Disorders in both the inpatient and outpatient setting.
Initiate treatment of common Movement Disorders that present in the inpatient and outpatient setting, including Movement Disorder emergencies.
Initiate treatment of common non-motor components of movement disorders
Discuss appropriate patients for surgical treatments of movement disorders
Recognize and distinguish functional movement disorders
Clinically classify abnormal movements by phenomenology: parkinsonism, chorea, tremor, dystonia, tics, ataxia, myoclonus and others
Construct a differential diagnosis for patients with each of the broad categories of movement disorders
Formulate a diagnostic strategy for patients with movement disorders
Describe non-motor components of movement disorders including behavioral, cognitive, autonomic and other features
Describe basic principles of neuroanatomy, neuropathology and neuropharmacology as they pertain to Movement Disorders
List side effects of common Movement Disorder therapies
Describe the indications for botulinum toxin injection therapy
Perform basic interpretation of common neurologic imaging studies of the brain and spine (MRI and CT) in patients with Movement Disorders
Schedule
The weekly assignment email will include the rotation schedule.
Movement Disorders Division meetings:
Every week Wednesdays 4-5pm: Didactics with Dr. Reich
Grand rounds auditorium
2nd Mondays 5-6pm: DBS meeting
Neurosurgical conference room, 12th floor main hospital
2nd Thursdays 4-5pm: Journal Club
Paca Pratt Conference room or ZOOM
4th Thursdays 4-5pm: Video Meeting
Paca Pratt Conference room or ZOOM
Readings
Treatment of Restless Leg Syndrome
Practice guideline update summary: Botulinum neurotoxin for the treatment of blepharospasm, cervical dystonia, adult spasticity, and headache
Evidence-based guideline: Treatment of tardive syndromes
Evidence-based guideline: Treatment of essential tremor
Continuum – Movement Disorders August 2019 (or most recent version if/when updated)
Last Updated: March 7, 2025