Orders Information for Admits, Discharges, and Other Treatments and Services
How to Admit
1. Under orders, type in “Neurology admission.” This will open an order set that you need to click through.
a. Under “Admission” select the level of care (IMC, floor) and the accepting team
b. Enter patient’s code status and anything else that has a red stop next to it
c. Ensure pt is kept NPO if needed (ex. facial droop or severe dysarthria)
d. Ensure that vital parameters (BP) are accurate
e. Ensure vital signs and neuro checks are ordered appropriately
f. Enter moderate to high risk VTE ppx: select heparin or lovenox and SCDs
g. Other useful order sets
i. Adult diabetes protocol- where you can find sliding scale
ii. Stroke order sets
1. Post tPA
2. No intervention
2. Med reconciliation
a. Find the ADT tab: click on Admission, “Order rec-Sign now”
b. Click through the tabs on the top- start with “review prior to admission meds”. Make sure this list is up to date, and delete anything the pt is no longer on
3. Find the ADT tab: click on Admission, “History Activity”
a. Click through the options on the left to enter PMH, family history, social history, etc
b. Once this is entered, you can right click and refresh these sections on your note for them to auto fill
ADMISSION TYPE: OBSERVATION VS ADMISSION
The general rule of thumb is that if a patient will be staying in the hospital for 2 midnights (including their time in the ED), then they should be admitted. If you anticipate that he will not be staying that long, then you should place them under Observation. Keep in mind that a patient placed under Observation can later be converted to an Admission. The opposite can also be done (Admission --> Observation), but is slightly more complicated.
How to Discharge
IF patient going to rehab: needs AVS + Discharge Summary + Discharge order SIGNED
IF patient going home: ONLY needs AVS + Discharge Order at time of dc
Steps to discharge
1. Go into ADT and click Discharge tab
2. Click on Order reconciliation
3. Within Order rec, click on “Reconcile medications” on top
4. Continue any home meds that were continued inpatient, add any new prescriptions
o When adding new prescriptions, can click “e prescription” to send directly to patient’s home pharmacy (must make sure the correct pharmacy is entered). This will not work for controlled substances.
o If you want paper scripts, click “Normal”
o If a patient is going to rehab, click “No print”
5. Sign order reconciliation once complete
6. Next click on Follow Up Providers within ADT Discharge tab. Add any follow up appointments the patient needs. For Neurology, simply type in “neurology” and Frenkl clinic should come up. BE SURE to EPIC message Lynette Goffin (residnet clinic) about needing an appointment so that it will actually be scheduled.
7. Next, complete the Gen Discharge order set for diet and activity orders. Select “continue current diet order” and “continue current activity order.” If the patient has a dressing that needs specific instructions, enter here.
8. Next click Patient Instructions. You can type in your own instructions here, and add patient education materials.
9. Next click “Preview AVS.” Make sure there is nothing in red on top of the after visit summary- this is how you know the ADT is complete.
10. IF patient needs home therapies: Consult to care management, home therapy. Check with case manager if a Face to Face note is needed.
11. IF patient needs outpatient therapies: place orders for “Ambulatory referral to *** therapy.” These will print out like scripts.
12. Finally, enter a discharge order that states where the patient is going and when
13. Once the above steps are complete, let the patient’s nurse know that the patient is ready for discharge.
14. Don’t forget your discharge summary if the patient is going home!
IF patient is going to rehab: please ensure that the med rec is inserted into the discharge summary. This can be done using the dot phrase “.avsmedslist”
How to Release MAR Hold Orders
1. Under the ADT tab, click on Transfer, “Order reconciliation”
a. Select “review current orders” on top, click “continue unselected”, click “sign and hold for accepting unit”
2. Then go to Manage orders, click on “signed and held” on top, “modify or release signed and held orders”. This will open up a pop up where you click on the left side on your orders, scroll all the way down and select continue all selected orders
How to Transfer
1. Enter order “Transfer patient”
a. Select the option to “transfer patient” if they are going to a difference service, or “change level of care” if they are transferring between floors (ex. IMC to floor)
2. Under the ADT tab, click on Transfer, “Order reconciliation”
a. Select “review current orders” on top, click “continue unselected”, click “sign and hold for accepting unit”
Cardiac Event Monitor
Place order: CAR14 event monitor enrollment. Be sure to specify indication and length of monitoring.
Call 86056 (EP lab) and give them patient info for enrollment.
IR Guided LP
Place order for IR guided LP
Page Neuro IR 11175 and discuss case/scheduling with fellow
IVIG
Typically used to treat AIDP, CIDP, or an autoimmune process. Use with caution in patients with CAD, stroke, renal disease, or hypercoagulable state as IVIG may increases hypercoagulability.
Dosing will be 2 g/kg divided over 2-4 days consecutive days versus 1 g/kg divided over 1-2 days (for patients with CIDP based on ICE trial). Always confirm dosing with attending.
Call inpatient pharmacy (8-5644) to help with inputting orders as there is a specific way they like to put it in your first go-around.
Moderate Sedation
Staff needed:
Nurse who is certified to monitor moderate sedation (most IMC nurses are),
Sedation provider (NP from CNS or NCCU)
Neurology resident
Patient must be IMC status
Physically on 4th floor
IMC status on 5th floor with appropriate staffing. Check with 5th floor charge nurse to ensure correct staffing. PolicyStat will state that patient must physically be present in IMC or ICU for this procedure to be done. I have been done told that this is not necessary as long as patient is IMC status under admission order and there is appropriate IMC staffing on the 5th floor.
MRI WITH SEDATION
Call 8-0231: Option 1 will get you to MRI Sedation Nurses
Ophthalmology Consultation Guidelines
Ophthalmic consultation is generally most appropriately provided at one of our outpatient clinical sites where we have access to our full range of examination and advanced diagnostic equipment. In-patient and ED ophthalmic consultations when necessary will be provided by our consult resident/attending during normal work hours. At other times, emergency and urgent consultations will be provided by the “On Call” ophthalmology resident.
Outpatient Scheduling can be arranged by phoning 667-214-1111
INPATIENT CONSULTATION (INCLUDES SHOCK TRAUMA AND ED)
Page the consult ophthalmology resident and provide the following information:
The name of the patient’s physician attending of record, and name of the patient
The patient’s diagnosis
Pertinent medical information including the specific medical indication/reason for the ophthalmic consultation
The exigency of the consultation: routine, urgent or emergency;
Routine, no immediacy, should be performed before the end of the next full workday.
Urgent, important patient diagnostic or treatment need, consult should be performed as soon as possible, certainly within a few hours.
Emergency, immediate risk to patient’s life or limb, consult should be performed straightaway, ideally within 1 hour, even if this requires calling in the second on call resident.
Patient’s current best visual acuity (patient should be tested using their current glasses on). Measure using a wall mounted Snellen chart when possible. Other alternatives include a “near vision card”, or one of the many available smart phone apps. Count fingers method is not useful.
Pupil exam (please check for afferent pupillary defect)
Extra ocular movements
Confrontation visual field findings
Description of optic nerve
GENERAL CONSIDERATIONS
Acute monocular vision loss.
Central Retinal Artery Occlusion is considered by the American Heart Association to be a stroke equivalent syndrome and if within 4.5 hours of onset (in selected patients up to 6 hours) should be treated as such. The Brain Attack Team is set up to rapidly treat acute strokes.
In patients within 6 hours of onset of suspected CRAO, an emergency consultation from Ophthalmology to rule out other causes of acute monocular vision loss is appropriate.
Papilledema evaluations.
A patient with a history of papilledema / IIH, with no acute change in symptoms or visual acuity, or a patient currently followed by Ophthalmology, rarely needs an emergency or even urgent consultation. These patients are more appropriately evaluated as outpatients.
Papilledema evaluations in the setting of a known history of pseudotumor cerebri or suspected elevated intracranial hypertension from other causes (such as Chiari malformation or intracranial mass effect) likewise rarely require an emergency or even urgent consultation. If an ophthalmology consultation is requested to aid in clinical decision-making, we are happy to provide consultation but the natural history of papilledema, detailed below, puts limits on the recommendations we can make:
Although the presence of papilledema is an importance clinical sign of elevated ICP, its presence or absence is not absolutely predictive of a patient’s current ICP status.
Patients with a history of chronic papilledema later often have atrophic optic nerves and no evidences of disc edema on exam.
Patients with chronic optic disc edema may not have acute changes or elevation in intracranial pressure.
Resolution of papilledema after medical or surgical management may take weeks or longer.
Optic nerve examination, especially without dilation, should be performed using the direct ophthalmoscopes located in all ED exam rooms, prior to calling for an ophthalmology consultation, and the finding reported to our consult resident who will later re-examine the patient. As this ophthalmology consultation may not occur immediately, neurosurgical or neurologic clinical decision-making should not be deferred pending our examination.
Pituitary adenomas (includes hemorrhagic). Patients with pituitary adenomas are often followed by ophthalmology with visual field studies. In the acute inpatient setting, obtaining an automated perimetry is rarely necessary or clinically useful. Our department Visual Field Consult policy details the limited situations in which ophthalmology will provide an inpatient Visual Field that are most appropriately perform in an outpatient setting.
Cranial nerve 3 or 6 palsies of known etiology with or without diplopia
Patients with cranial nerve 3/6 palsies (old or new) of known etiology should see a neuro-ophthalmologist in the ambulatory setting within 4 weeks after discharge for full a comprehensive ophthalmic evaluation.
In the acute setting in an adult, diplopia may be managed with patching one eye. Vision corrective lenses, including prism lenses cannot be measured, prescribed, provided or fitted on inpatients. In addition, for patients whose diplopia is new or changing, the proper treatment cannot be determined. The proper treatment can only be determined after the condition has fully stabilized which may take many weeks and may require referral to an ophthalmology strabismus specialist.
Ordering a Sleep Study
There is a smart-phrase in EPIC to put the STOP-BANG questionnaire into your note. It is titled .CPKSTOPBANGSLEEP. You can also create one by copying and pasting the STOP BANG questionnaire below.
STOP-BANG Sleep Apnea Questionnaire
STOP
Do you SNORE loudly (louder than talking or loud enough to be heard through a closed door?
Do you often feel TIRED, fatigued or sleepy during the daytime?
Has anyone OBSERVED you stop breathing during your sleep?
Do you have or are you being treated for high blood PRESSURE?
BANG
BMI more than 35 kg/m2?
AGE over 50 years old?
NECK circumference > 16 inches (40 cm)?
GENDER: Male?
Interpretation:
3 or more YES answers indicates moderate to high probability for obstructive sleep apnea. Consider ordering diagnostic sleep studies as appropriate. Sleep clinic referral may be requested following studies.
Guidelines on how to order a sleep study by Dr. Steven Scharf, director of the sleep program at UMMC:
To order a sleep study, you can do this in one of 2 ways.
Fill out a paper form (must be signed by an attending). Fax it to our office: 410-706-0345. I usually recommend having the patient speak with the office to schedule the study: 410-706-4771. A big problem is that many insurance providers are requesting prior authorization to perform sleep studies in the lab. They are wrong, but they think this saves money - it does not. Usually, having had a stroke is a reason not to do a home study. However, we will leave enough time to obtain the authorization. If authorization for a diagnostic study is denied (a common problem), we will change the order to a SPLIT study (start as diagnostic, switch to CPAP IF the initial severity is bad enough - usually it is not). Sorry, we have to conduct our business like this.
In EPIC go to orders, type in polysomnography. You will get a list of 3 things. The first one is the only legitimate one as it is the one I had put together. It is for diagnostic study only. Fill it in, print it out and FAX it to us (it does not magically appear in our office). The other 2 are some generic orders that appear in EPIC and have nothing to do with us.
Please remember that all orders (the paper one OR the EPIC one) have to be faxed to the office at 410-706-0345.
PICC Access
If lines are not emergent and can wait for normal PICC team hours please contact the UMMC PICC team during daytime hours.
A company has been hired by the hospital for urgent/emergent lines after 4pm until 11pm, holidays and weekends. APS will use the same equipment and place the same PICC as done by the UMMC PICC team.
To place order for PICC enter "IR PICC by non-physician" in EPIC and inform the patient's nurse of reason for urgency.
Nursing will call the Rapid Response / ExpressCare Coordinator, who will contact the Advanced PICC Services.
The number for the rapid response coordinator is 8-3011, this number can be called M-F day or night.
On weekends, call 8-1234 the ExpressCare communication center.
Plasma Exchange on the Floor/IMC
This is done through Hematology (consent to be obtained by Hematology). Usually done every other day, sometimes consecutive days if patient tolerates well. This is not done on weekends.
Obtain PLEX catheter (Consent is obtained by provider performing the procedure). 3 options are:
NP (CNS or NCCU)
ACES (During day hours 7 AM - 5 PM)
MICU Fellow (After hours 5 PM - 7 AM. x8-6196 ask for fellow)
Consult to Heme/Onc for plasmapharesis. They will provide a Nurse.
On days of PLEX, utilize the UMMC Plasma Exchange Supplemental order set (type “plasma exchange” into order set search box)
Be sure to order pre- and post-PLEX labs including full panel of electrolytes and coag panel.
Pre-PLEX labs need to be done earlier or they will not perform the PLEX.
Order the vital signs associated with the order set during PLEX. Make sure they are on cardiac monitoring
Be sure to order the heparin flushes on off-days and on-days to prevent stenosis.
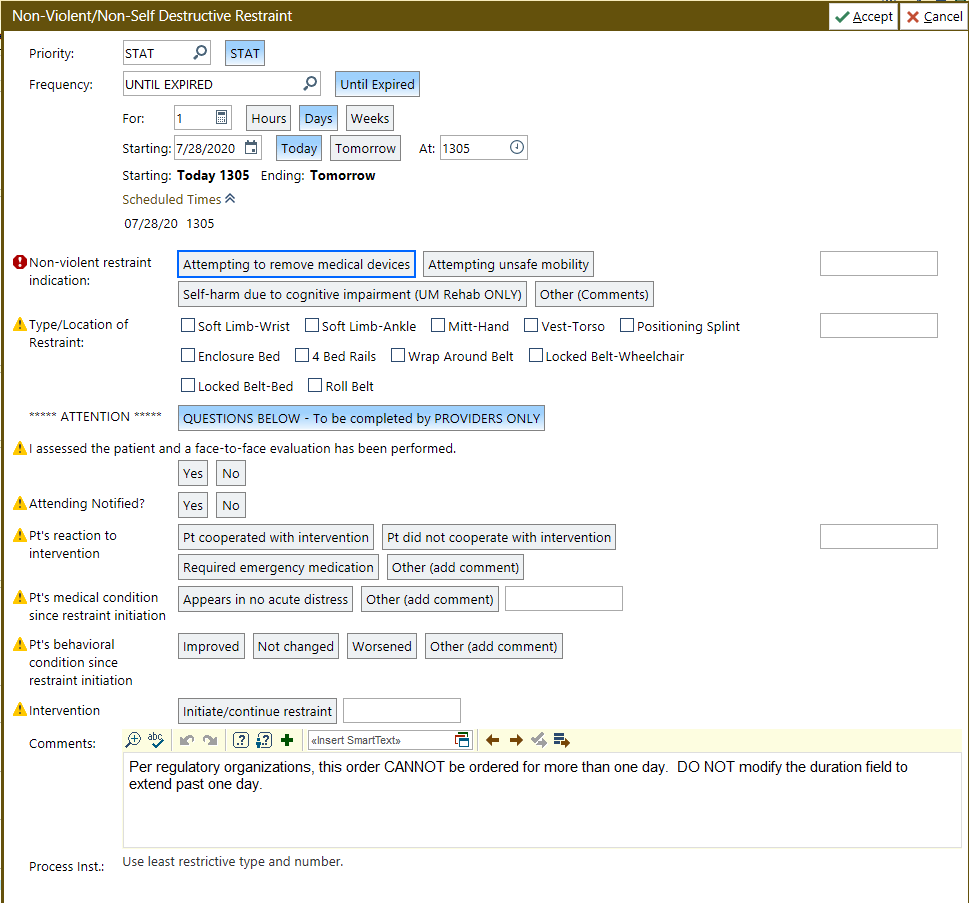
Restraint Initiation and Renewal
A few important points:
Every question MUST be answered, including all the yellow triangle questions when you initiate OR renew restraint orders
You need to go see the patient if nursing is asking you to initiate restraints or add additional restraints.
New restraint orders MUST be placed and time stamped within 15 minutes of when the nurse initiates them. It is good practice to confirm with him/her the official start time so you're on the same page with documentation.
Daily renewals can be done after pre-rounding or rounding on the patient so you can truthfully answer the 'face to face' evaluation question
For new or additional restraint orders, just DocHalo the attending on record and answer 'Yes' to the 'Attending Notified' question. For renewals, you will round with the attending, so she/he will be aware.
Restraints just need to be renewed each calendar day, so if you are called while on night float after midnight to renew restraints, it is perfectly reasonable (and easier) for you to sign this out to the oncoming team.
Seniors, please make sure you are reviewing these orders and ensuring they are done correctly by junior residents and psych interns.
Below is an example of the order with all the questions that need to be answered.
Rituxan Authorization for Continued Outpatient Therapy
Rituxan infusions are done as an outpatient through the Stoler Infusion Center. The Frenkil Clinic will not attempt these infusions unless they have received infusions from Stoler with no complications.
Depending on availability, staff from the Neuroimmunology department may be able to assist with this. Please check in with Dr. Benavides, Dr. Rus, and Dr. Harrison on a case by case basis.
Steps to arrange Rituxan order:
Bonnie Iler, Nurse who reviews the orders, is in the Stoler Pavilion in rm N1W71, next to the A-wing conference room, and available to help.
Written Cytoxan order:
Obtain from Stoler Infusion center OR
Print from Intranet: UMMC Insider>Depts & Services>Depts A-Z >Cancer Order System (ICOS).
Resident can fill it out but it needs to be signed by and attending.
Copy of the consent unless it’s already scanned in the patient’s chart.
Published article referencing the dosing for the specific disorder being treated.
Send message to Stoler Off Service Infusion Pool (#201831) via Epic staff message.
Use Smartphrase: .stoleroffservicerequest (Stoler off service request) (it is extremely lengthy so be prepared…)
All details must be included in order for our team to properly schedule the patient. The sender will be notified when the patient has been scheduled. Please allow up to 1 week for scheduling
Sleep Promotion
These new guidelines are active and available in PolicyStat
There is a corresponding order and order set that the provider can use to individualize sleep promotion
Includes a door sign that clearly defines the uninterrupted sleep period
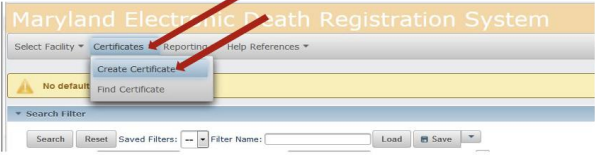
Maryland Electronic Death Registry
1. Start by creating a new certificate and enter the patient’s demographic information.
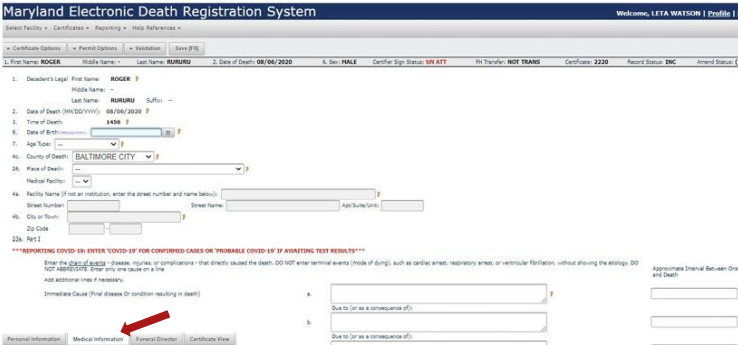
2. The only part you are responsible for filling in are the boxes under the “Medical Information” (MI) tab. This includes place of death, cause of death, and contributing causes.
TIPS:
- If the Manner of Death is “Natural”, as it is with most of our patients, items 28a-28g can be skipped.
- “Approximate interval between onset and death” and “Contributing Causes” are both required fields. If there is nothing to report or it’s unknown, enter a hyphen (-) or “UNK”.
- Avoid using “cardiac arrest” as the immediate cause of death. Instead consider more specific conditions such as “hypoxic respiratory failure” or “septic shock”.
- Be sure to spell out any common abbreviations (ie. DM= Diabetes Mellitus)
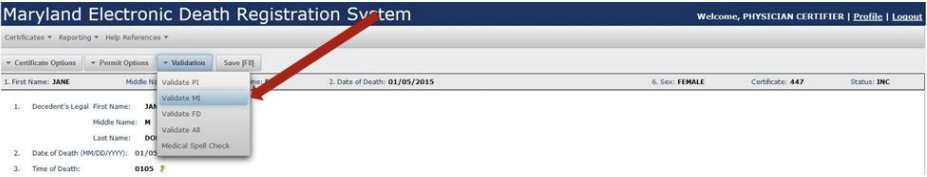
3. Next, you ask the system to validate the medical information you inputted. Any missing data or spelling errors will be listed at the top of the page in red.
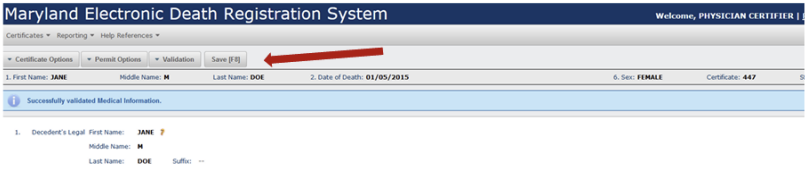
4. After the MI is successfully validated, then you can save your work by pressing the “save” button.
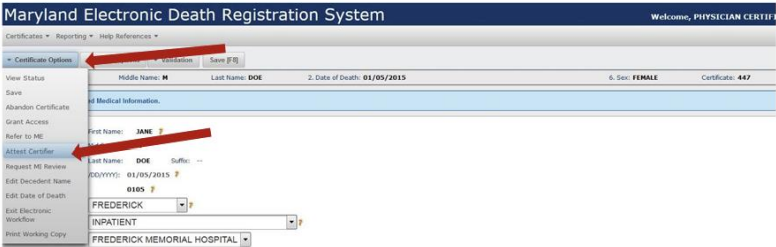
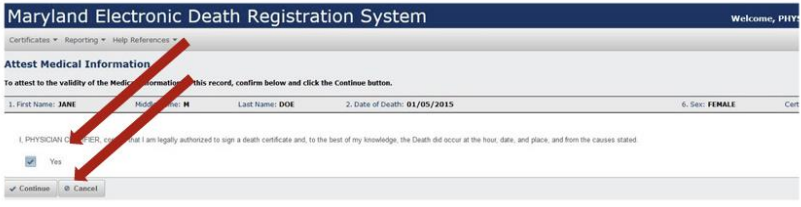
5. Once the MI is saved, you still need to attest the certificate in order to sign it. After you click “Attest Certifier”, check the box for “yes” and click continue. Congratulations, the certificate is now signed and locked!
TIPS:
- Any provider can attest a certificate so there is no need to defer to an attending or fellow.
- Rotators from other hospitals may not have access to EDRS. If that is a case, they must ask another member of the team to complete the certificate ASAP.
- If you have forgotten your account log in, you can request your username and password from your program coordinator or email edrs.help@maryland.gov.
- If you need to adjust a certificate after it has been signed, you can unlock it by selecting that button under the “Certificate Options” menu. Remember the certificate will need to be signed again after your edits are complete.
Please complete the death certificate as soon as possible in order to expedite the release of the deceased to the funeral home/families
UmmSafe Reporting
See this powerpoint for step-by-step instructions on how to enter a report.
The down and dirty of UMMSafe:
If you’re thinking “should I enter this in UMMSafe” you probably should. (not a venue for blame just facts of the event)
It’s used to track systemic issues and trends.
To open UMMSafe- There is a link on the INTRANET home screen under staff quick links called “UMMSafeEvent Reporting” (see PowerPoint)
Login- Use “UMMS” as log in venue- Username and password- same as EPIC
The next step is the hardest task. A screen of 20 possible scenarios will populate. Pick the one that is closest related to the event you want to report. Use your best guess. Don’t be discouraged by this step. If it is wrong classification, risk will fix it internally after submission.
Final step is to fill out the report- There will be anywhere from 11-18 mandatory fields which is dependent on the scenario you choose.
Report the facts only- Someone from risk/legal will reach out for more details if needed.
VA Transfers
Contact Linda Moses: 410-605-7433. She will determine if there is bed availability. If there is then and only then should you present patient to accepting medical team. You need to check everyday. Supervisor there is Sandy Jones: 410-605-7000 (3672). Main hospital number is 410-605-7000.
Last Updated: September 2, 2024