Inpatient Services’ Schedule and WorkflowSchedule
Efficiency Strategies
Residents are expected to pre-round on the patients and have data on interval events and test results ready for rounds (Not “Discovery Rounds”).
Watch the Clock – goal ≤ 10 min per established patient
Agree to come back for more lengthy conversation with family if needed
Having a direct number to RT, PT/OT/SLP and Pharmacy may be an alternative to having them on rounds so we can get help from them in real time.
If orders are placed, talk to therapists and Tiger message consultants during rounds. This way plans can be put into action sooner.
If the service is especially busy and rounding needs to continue beyond the usual morning time, the attending and senior resident will determine the most efficient plan (e.g. Attending and senior take med students to see remaining patients while junior residents do work/see new consults; Attending goes with one resident at a time to see their patients, etc.)
Keep track of patient measures on the whiteboard every day to check on tasks and to get a change to debrief about rounds.
Medical Students
Medical students should carry at least 2 patients each and be fully responsible for daily case presentations.
Communication with the family should be a daily event by someone from the team. Medical students are particularly good at this task and should be instructed to answer what questions they can and promise to find answers to those they don’t know. It is expected that attending physicians will speak to families during the hospital stay.
Attending Daily Tasks
Sign admission orders daily
Review and cosign progress notes/H&Ps/Consult notes daily
Patients Accepted for Transfer from OSH
Attending:
Call senior residents on service or resident on call to tell them about patient
Write a ‘Documentation Only’ note in EPIC with the details from the initial call
Follow-up on patient status through MEC if questions arise as to whether pt remains appropriate for transfer
Senior Resident:
Place patient on Pending Patient list in Epic
Review pending neurology transfers report in Epic at the beginning and end of day to make sure there are no additional patients there who are not on the pending patient list.
Check the timeline for notes from MEC. Remove patients from pending list if transfer canceled.
Sign out pending patients to call resident
Nurses will page resident when they are notified that bed is available/when they receive report.
If concerns arise regarding whether the patient remains appropriate for level of care (based on Epic review or nursing report), notify the attending on-call who can follow up with the sending provider through MEC.
Pending Patient Workflow
Clinical updates on pending patients:
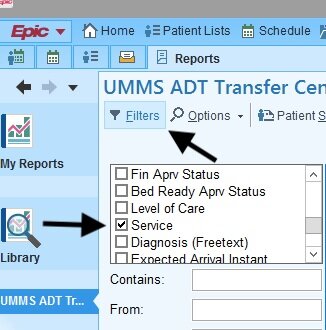
In order to view Transfer list:
Go to My Reports on top of EPIC toolbar
Click on "Library"
3. Type in "UMMS ADT transfer center all active requests." Make sure nothing is checked off under "Types" on the right side of the window.
4. Click "Run"
5. Patient list will appear - on top left, Filter by specialty and click Neurology
6. This should show you all pending neurology transfers, what unit, accepting provider. In the bottom half of your EPIC window, you can see a timeline of when the pt was accepted and clinical updates.
CNS senior will check Transfer list every morning and prior to sign out
CNS senior responsible for signing out any patients pending transfers to short call
General Neurology Inpatient and Consult Attending Call schedule
Attending blocks start on Fridays for 7 days
Call shifts are from 8AM to 8AM (i.e. Attending listed under Monday starts the call shift Monday morning at 8AM and finishes Tuesday morning at 8AM)
The weekend coverage assignments are set to optimize patient coverage continuity so that either the attending or the senior resident will be present for both the inpatient and consult teams each weekend (i.e. the Inpatient attending is on the weekend with the Consult PGY4 and the Consult attending is on the weekend with the Inpatient PGY3). For this reason, weekend call swaps are discouraged.
Last Updated: November 19, 2024